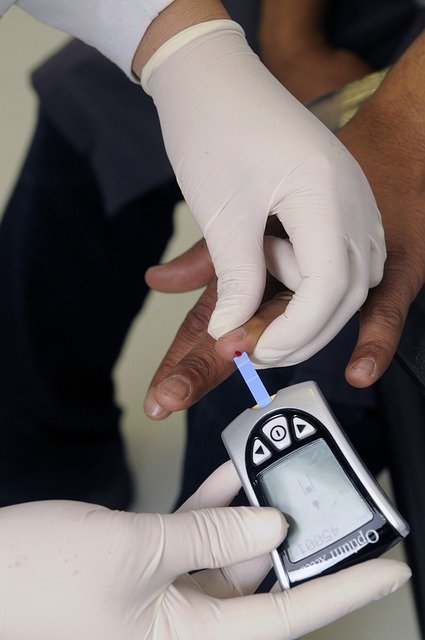
Understanding A1c Levels: A Comprehensive Guide to Blood Sugar Testing
A1c levels provide healthcare professionals with a vital window into long-term blood sugar control, offering insights that extend far beyond what daily glucose monitoring can reveal. The hemoglobin A1c test, commonly referred to as HbA1c or simply A1c, measures the average blood glucose levels over the past two to three months by examining how much glucose has attached to hemoglobin proteins in red blood cells.
What the A1c Test Measures Compared to Daily Glucose Checks
The fundamental difference between A1c testing and daily glucose monitoring lies in their timeframes and scope of measurement. Daily glucose checks provide a snapshot of blood sugar levels at specific moments throughout the day, capturing immediate fluctuations caused by meals, exercise, stress, or medication timing. These readings offer valuable real-time data but can vary significantly based on temporary factors.
In contrast, the A1c test measures the percentage of hemoglobin proteins that have glucose molecules attached to them. Since red blood cells live approximately 120 days, this test reflects average blood glucose levels over the preceding two to three months. The A1c result is expressed as a percentage, with normal levels typically falling below 5.7 percent for individuals without diabetes.
This longer-term perspective makes A1c testing particularly valuable for assessing overall diabetes management effectiveness. While daily glucose readings might show excellent control on testing days, the A1c can reveal whether blood sugar levels have been consistently managed over time or if there have been periods of poor control that daily testing might have missed.
Situations Where A1c Testing is Commonly Included in Health Exams
Healthcare providers routinely incorporate A1c testing into various medical examinations and screening protocols. Annual physical examinations often include A1c testing for individuals over 45 years of age or those with risk factors for diabetes, such as obesity, family history, or sedentary lifestyle patterns.
Diabetes diagnosis protocols frequently utilize A1c testing as a primary diagnostic tool. The test offers convenience over traditional glucose tolerance tests since it requires no fasting or special preparation. An A1c level of 6.5 percent or higher on two separate occasions typically indicates diabetes, while levels between 5.7 and 6.4 percent suggest prediabetes.
For individuals already diagnosed with diabetes, A1c testing becomes a regular monitoring tool, typically performed every three to six months. Healthcare providers use these results to evaluate treatment effectiveness and make necessary adjustments to medication regimens, dietary recommendations, or lifestyle interventions.
Pregnancy care often includes A1c testing, particularly for women with risk factors for gestational diabetes or those with pre-existing diabetes. The test helps healthcare providers assess blood sugar control during pregnancy planning and throughout gestation periods.
Factors That Can Influence A1c Results Over Time
Several physiological and medical conditions can significantly impact A1c accuracy and interpretation. Anemia, particularly iron-deficiency anemia, can artificially lower A1c results because reduced red blood cell counts affect the calculation basis. Conversely, conditions that increase red blood cell lifespan may elevate A1c readings beyond actual glucose control levels.
Kidney disease can influence A1c results through multiple mechanisms, including altered red blood cell production and changes in glucose metabolism. Individuals with chronic kidney disease may experience falsely elevated or decreased A1c levels depending on the specific kidney function impairments present.
Hemoglobin variants, which are genetic variations in hemoglobin structure, can interfere with certain A1c testing methods. These variants are more common in individuals of African, Mediterranean, or Southeast Asian descent and may require alternative testing approaches for accurate results.
Recent blood loss or blood transfusions can temporarily affect A1c accuracy since the test relies on red blood cell glucose exposure over time. Significant blood loss removes older cells that carry glucose history, while transfusions introduce cells with different glucose exposure histories.
Certain medications can also influence A1c results. High-dose vitamin C supplementation, some antibiotics, and medications affecting red blood cell production or lifespan may impact test accuracy. Additionally, conditions causing rapid red blood cell turnover, such as hemolytic anemia, can produce misleadingly low A1c results.
Age-related changes in red blood cell metabolism and lifespan can gradually influence A1c interpretations over time. Older adults may experience slightly different A1c patterns compared to younger individuals, even with similar glucose control levels.
Understanding these influencing factors helps healthcare providers interpret A1c results accurately and determine when additional testing methods might be necessary. For individuals with conditions affecting A1c reliability, alternative monitoring approaches such as fructosamine testing or continuous glucose monitoring may provide more accurate assessments of long-term blood sugar control.
The A1c test remains a cornerstone of diabetes management and diagnosis, providing valuable insights into long-term glucose control patterns that complement daily monitoring efforts. Regular A1c testing, combined with understanding of factors that may influence results, enables more effective diabetes management and better health outcomes over time.
Disclaimer: This article is for informational purposes only and should not be considered medical advice. Please consult a qualified healthcare professional for personalized guidance and treatment.




